ADHD—What Foster Parents Need to Know
Eight percent of children in foster care in Washington State have a diagnosis of attention-deficit/hyperactivity disorder (ADHD) at the time they enter foster care. Even more children receive a diagnosis after entering foster care and receiving consistent medical care, sometimes for the first time in their young lives. So odds are good that you will care for a child managing the symptoms of ADHD at some point during your foster parenting career. So let's talk about ADHD—what it is, how it's typically treated, and what parents need to know about parenting a child with ADHD.
What is ADHD?
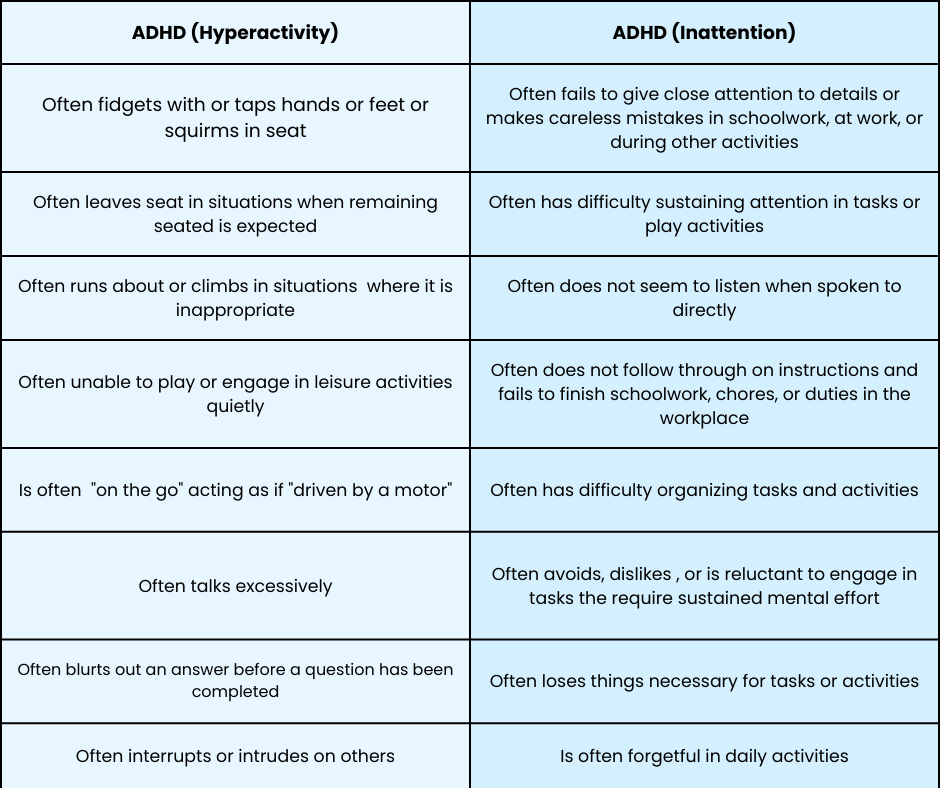
The Diagnostics & Statistical Manual (DSM) published by the American Psychological Association (APA), now in its fifth iteration, lists two eight symptom lists of which at least six must be present in order to render an ADHD diagnosis. The two lists correspond to the two different types of ADHD—hyperactive & inattentive (see above chart).
While a mixed presentation is possible (and common, actually), in many ways the two variations are opposites. Hyperactivity is an externalized condition with highly physical symptoms while inattention is a more internal condition with psychological or emotional symptoms. Hyperactivity presents as too much of something (energy, enthusiasm, friendliness, or physicality), and inattention presents as too little of something else (focus, motivation, listening, or endurance).
For foster parents though, the most important thing to know on this subject is that: a response to trauma can be easily confused with the symptoms of ADHD. In fact, "problems with concentration" is one of the symptoms of Acute Stress Disorder (ASD) the most common diagnosis for children dealing with a traumatic past. Other possible symptoms for ASD include hyper-vigilance (which could be the reason a child has difficulty sustaining attention or seems not to listen when spoken to), an exaggerated startle response (which might lead a child to blurt out an answer or interrupt), irritable behavior (which might look like a child climbing or running about). In fact, all but one symptom (sleep disruption) of ASD pairs neatly to the possible symptoms of ADHD. So the two things are very easily confused.
Even without a traumatic past, diagnosing ADHD in children is very hard to do accurately. According to the APA, a best practice diagnosis requires the synthesis of multiple types and sources of information gathered from multiple reporters in a variety of modes and settings. An ADHD diagnosis may involve assessments, like:
A symptom questionnaire filled out by both the child and some adults in their life, like teachers and/or parents
An interview of both the child and their caregivers
Some direct observation in the situations where ADHD symptoms have been challenging like a classroom
An exercise called a Continuous Performance Test (CPT)
A direct measurement of brain activity using a Quantitative Electroencephalogram (qEEG)
If a diagnosis is rendered after just one of these things (a questionnaire for example) be very suspicious of the results, particularly if there was little exploration of a child's history.
How is ADHD treated?
Medication
The most common treatment for ADHD is prescription amphetamine stimulants, which might seem counter-intuitive especially for the hyperactive. But in a biological sense, attention deficits are often caused by a reduced capacity for filtering stimuli in the mid-brain. And stimulants can enhance the functioning of that filter, resulting in behavior stabilization.
However, there are three notable downsides to be aware of. First, amphetamines are highly habit forming. Second, other biological structures can cause attentional deficits too and amphetamine stimulants are less effective in treating attentional deficiency caused by those things. Unless the diagnosis included a qEEG, prescribing an amphetamine like Adderall or Ritalin is done as a best guess. Finally, medications of this type have an intense spike/crash effect in which the period after the active ingredients have burned off, can result in even worse mood & behavior for a child than they exhibited prior to medicating.
Amphetamines can be a very helpful treatment for many children suffering from attentional deficits, and it’s important to weigh various options and decide what’s best for the child.
Mindfulness
Mindfulness is gaining notoriety as an ADHD treatment, used both to augment and replace stimulant medication. Mindfulness is a psychological intervention in which a child is trained to be aware of themselves, their body, their mood/mindset, and surroundings through exercises like focused breathing. While it doesn't seem like much, the efficacy data is quite strong that with greater mindfulness comes better impulse control and stimuli filtering. Over time these exercises can teach children to set, sustain, and adjust their attention on their own.
Neurofeedback
Neurofeedback has also emerged as a gold standard treatment for ADHD, proving as effective as medication in reducing the symptoms of attentional deficits in children as young as eight. Neurofeedback is a lot like mindfulness, except that a device is used to measure a child's brain activity and that information is translated into a video game-like experience in which the child is rewarded when they are paying close attention to the game, but not if their mind wanders from the tasks they are assigned in the game. Much like mindfulness, this is exercise so it takes time to see an effect, but has produced great results (without any side effects) for kids who stay with it.
Advice for (foster) parents of an ADHD child.
Get a thorough best-practice diagnosis from a psychologist.
Given how common it is, there's a lot of armchair diagnosis of ADHD. Social workers, teachers, school counselors—people who know a lot about kids and can make a pretty strong guess about which kids struggle with attention—can give you a good first impression. But if you have reason to suspect that attentional deficit is part of your child's experience, you really should see a specialist—ideally a psychologist or other mental health professional who can deliver a formal diagnosis using a combination of instruments (qEEG, CPT, and symptom questionnaires in combination, for example).
Mix and match treatments to find what works for your child.
Amphetamine medication might help your child a lot, but don't rule out some of the emerging alternatives. These things can be used in addition to medication and you may find that the best results come with 2 or 3 things in combination. Of course, work with your child's mental health provider to build the treatment plan.
Find your people.
Parenting a child with ADHD can be hard, but a lot of people do it. Be on the lookout for families who share your values and have done what you're trying to do. Make some friends even if just to remember that you're not alone in all this.
Sources and further reading:
Peak Mind: Find Your Focus, Own Your Attention, Invest 12 Minutes a Day
Mindfulness for Adult ADHD: A Clinician's Guide
Managing ADHD in School: The Best Evidence-Based Methods for Teachers